Intra-Beat Biomarker For Accurate Blood Pressure Estimations
Brief Description
Researchers at UC Irvine have developed a novel algorithm that more accurately filters raw blood pressure (BP) data collected from continuous non-invasive blood pressure sensors. The algorithm features improvements in eliminating baseline signal drift while maintaining signal integrity and BP estimation accuracy across significant hemodynamic changes.
Suggested uses
-Continuous, non-invasive blood pressure monitoring
Features/Benefits
·Improved cardiovascular outcomes for OR/ICU patients
·Single-sensor BP monitoring
·Validated in demographically and medically diverse cohort of 15 OR patients
·Reliable with stress- and drug-induced hemodynamic perturbations for as long as 20mins. without calibration
Full Description
The gold standard for blood pressure monitoring is the invasive arterial catheter (A-line) placed in a peripheral artery, but its use comes with the risk of several medical complications and is thus often reserved for the most at risk patients. Continuous non-invasive blood pressure (CNIBP) monitoring technologies have been developed to circumvent this, but they face significant drift and noise issues, require frequent recalibration, or have been shown to misperform in different clinical contexts (i.e. those with sudden hemodynamic changes in response to stress or drug administration). Wearable capacitive pressure (CAP) sensors have grown increasingly popular due to their convenient form factors, high spatial resolution, quick response times and low power consumption, but these devices are still highly susceptible to baseline drift. Since recent studies have correlated continuous BP patterns with cardiovascular outcomes, there is a pressing need for CNIBP monitoring technologies that are accurate across clinical contexts.
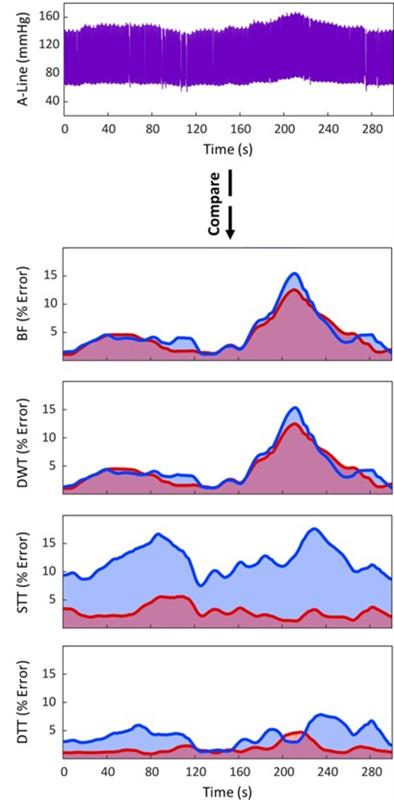
Researchers at UC Irvine have developed a new intra-beat biomarker they coined Diastolic Transit Time (DTT) that achieves highly accurate BP estimations. The novel algorithm used to capture DTT enables single-sensor BP monitoring, an improvement from previous algorithms that required multi-sensor data. The algorithm is significantly more accurate than its predecessors (BF, DWT, and STT), particularly in instances of greater BP change when compared to the A-line (see figure). When again comparing to the A-line, it was able to estimate BP accurately and precisely from multiple sensor types (CAP and photoplethysmography, PPG) across a wide hemodynamic range (Pearson coefficients of 0.987, 0.960, and 0.980 for systolic blood pressure, diastolic blood pressure, and mean arterial pressure, respectively; CAP sensor data). CAP sensor collected data filtered using the algorithm also agreed well with caretaker measurements on individuals who exhibited common arm/hand movement and on individuals who walked. As the demand increases for wearable biomonitors, this CNIBP monitoring technology excels in accuracy and precision, particularly in the context of hemodynamic change induced by stressors, drug administrations, or motion artifacts.
State Of Development
In vivo studies
Related Materials
Patent Status
Patent Pending
Contact
- Alvin Viray
- aviray@uci.edu
- tel: View Phone Number.
Inventors
- Khine, Michelle
